25 years of BioNews
Throughout 2024, PET will be celebrating the 25th birthday of BioNews. BioNews launched as a weekly digital publication in March 1999, and today we are publishing our 1225th edition...
Throughout 2024, PET will be celebrating the 25th birthday of BioNews. BioNews launched as a weekly digital publication in March 1999, and today we are publishing our 1225th edition...

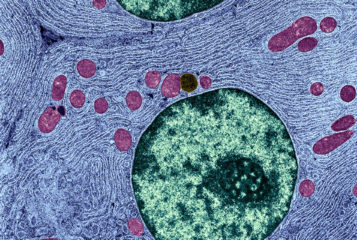
Luke Steventon reviews a radio programme about mitochondria, which are described as producing energy production levels of '30 million volts per metre – like a bolt of lightning'...
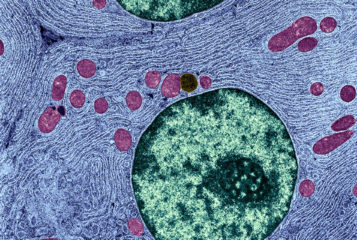
The birth of the first UK child(ren) with donated mitochondria has been confirmed by the Human Fertilisation and Embryology Authority...
by Sandy Starr
As mitochondrial disease and mitochondrial donation hit the headlines, PET clears up misunderstandings with its 'Mythbusting Mitochondrial Donation' resource, and with a set of recommended videos...
by Julia Chain
Scientific development is starting to push against, or go beyond, the boundaries of what is permissible under UK fertility law. It is time to modernise the law, and the HFEA has launched a consultation to determine how best to do that...
To kick off 2023, PET has asked ten key experts and advocates – working in the UK, the USA, Australia and Singapore – to tell us what they need us to do this year. Their responses have left us in little doubt that PET is needed now more than ever...

by Professor Catherine Mills and 1 others
Professor Catherine Mills and PhD candidate Ezra Kneebone from Monash University, Australia discuss the critical shortages of eggs available for fertility treatment and put forward a proposal to counteract this shortage, for both reproductive and research purposes...
by BioNews
This film documents a PET event about current legal limits on reproductive technology, and whether these limits should be changed....

Australia recently passed legislation explicitly allowing mitochondrial donation...

by Karinne Ludlow and 1 others
In this commentary, we consider the road to legalisation in Australia, the key aspects of this legislation, and some remaining unanswered questions...
BioNews, published by the Progress Educational Trust (PET), provides news and comment on genetics, assisted conception, embryo/stem cell research and related areas.

