Over the last 30 years I have met some remarkable families, from whom I have learned about the rewards and challenges of caring for relatives with incurable genetic conditions.
Perhaps the two most difficult things to tell a family are firstly, that there is no cure for the condition that affects them or their child; and secondly, if they plan to have another baby, that it will inevitably also be affected.
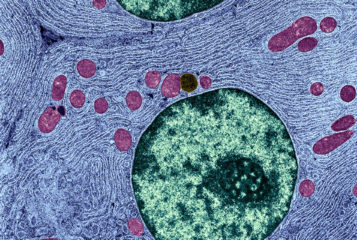
Mitochondrial conditions are notoriously hard to diagnose, because they present in so many different ways. Mitochondria are the tiny, but essential, energy-generating structures in our cells. Failure of the mitochondria has devastating effects on organs that need lots of energy to function: the brain, heart, kidneys, muscles and liver. Mitochondrial disorders are inevitably progressive, causing seizures, deafness, blindness, heart failure and liver failure. Affected individuals may die in infancy or childhood, and rarely survive into adult life.
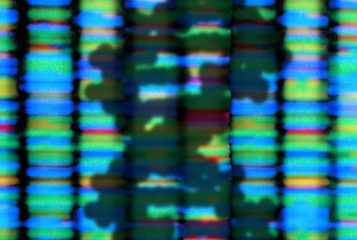
Mitochondrial disorders can be inherited in two different ways. The more conventional form of inheritance involves mutations in DNA in the cell nucleus. For families affected by this type of disorder there is a 1 in 4 risk of recurrence — conventional autosomal recessive inheritance. For these families, prenatal diagnosis (PND), or preimplantation genetic diagnosis (PGD), may be acceptable reproductive options if they wish to try and minimise the chance of having another affected child.
The second type of inheritance is very unusual and involves mutations in the mitochondria's own DNA. Uniquely, we all inherit our mitochondrial DNA (mtDNA) solely from our mothers — there is no paternal contribution. That means that if a mother carries high levels of mutated mtDNA, then all her children will inevitably inherit the mutation and will be affected. Such women will never have a healthy baby, unless novel techniques are introduced.
Prevailing scientific opinion states that mitochondrial donation is not unsafe. It employs techniques that have been the subject of 30 years of research in animals, and more than five years of research in human embryos. The safety of mitochondrial donation has been assessed in exhaustive detail in three expert scientific reviews convened by the Human Fertilisation and Embryology Authority (HFEA).
So how would the new treatment work? Essentially, IVF techniques would be used to replace the mother's faulty mitochondria with healthy mitochondria that have been donated, altruistically, by another woman. This could take place just before fertilisation (so-called maternal spindle transfer) or immediately afterwards (pronuclear transfer).
The draft Regulations don't allow these techniques to be used - rather, they permit the HFEA to consider applications for licences for treatment. This is an important distinction: if the draft Regulations become law, it does not follow that the HFEA will grant licences imminently or indeed at all. The HFEA will consider whether the proposed activity is safe, and whether the applicant has the necessary staff, expertise, skill and equipment. The draft Regulations simply allow this further review process to begin.
Conceiving a child via mitochondrial donation involves biological material from three people - the child's parents, plus a female mitochondrial donor. That is why these techniques are sometimes referred to as 'three-person IVF'. But that phrase, so beloved of the tabloid press, is really rather misleading.
We all have around 25,000 genes in the nuclei of our cells — and just 37 genes in our mtDNA. The mitochondrial genes make no significant contribution to any definable characteristics. So we are talking about a very tiny proportion of our total DNA (< 0.1 percent), yet one which plays a vital role in energy production. The amount of material involved is a minute fraction of the amount involved when someone has a bone marrow transplant or a kidney transplant, and yet we never sensationally refer to those patients as having four genetic parents even though their body contains DNA representing all 25,000 genes from four different people.
Many years ago I worked on a paediatric renal ward looking after children with kidney transplants, and I used to think about the courage of the doctors and patients who were involved in the first transplant. That was a brave step to take — and certainly one that could not be guaranteed to be completely safe. Even nowadays, as part of the consent process prior to transplant, we carefully discuss the pros and the cons of surgery before patients decide whether or not to proceed.
For the last 20 years, I have been involved in our PGD programme. Couples who have a high risk of conceiving children with a serious inherited disorder may choose PGD in order to allow embryo biopsy and genetic testing prior to the selection of an unaffected embryo for replacement into the womb. This treatment was introduced following far less scrutiny of the technology than is the case with mitochondrial donation.
Claims about the safety of proposed new therapies often serve as a convenient proxy for the ethical objections of people who are in fact more fundamentally opposed to mitochondrial donation.
If we are to offer mitochondrial donation, it will be essential that we counsel couples carefully and non-directively about the potential risks, as well as the benefits, and allow them to make their own decision. We cannot guarantee that treatment will be safe, any more than this is possible for other interventions; but we can tell couples that we have no evidence that treatment will be unsafe. We can, and must, insist that they allow us to follow up any children born following treatment, so that we can collect long-term outcome data. With the regulatory environment that exists in the UK we are uniquely well placed to do this.
Much of what is proposed differs little from other IVF techniques, but there is one important difference. The donated, healthy mitochondria will be passed on to future generations if the treated embryo is female.
I think that it is very important to understand the profound feelings that drive some couples to want to have children that are genetically related to them against all odds. Every couple is different and in our society, within reason, we allow people to make their own choices, even if, sometimes, they chose a path that others would not follow.
I do not for one moment want to minimise the concerns that introducing new regulations could engender, but I think that the responsible way to address these is to allow very carefully controlled and regulated treatment to take place in centres of excellence here in the UK, rather than allowing other countries where there is little or no regulation to take the lead.
Our duty of care means that we must strive to find the best possible treatments for our patients. Here in the UK we could lead the world with mitochondrial donation.




Leave a Reply
You must be logged in to post a comment.