A stem cell model has been developed to highlight the route of infection of the brain by SARS-CoV-2, the virus that causes COVID-19.
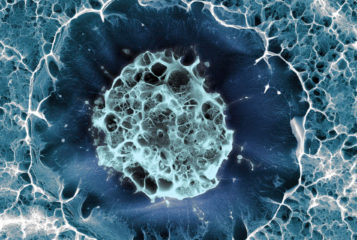
Pericytes are multi-functional cells that wrap around blood vessels, and they carry the ACE2 receptor that SARS-CoV2 uses to infect cells. US researchers introduced these cells to stem cell-derived brain organoids to create 'assembloids', a sophisticated stem cell model of the human body, which contains many types of brain cells, including pericytes, to model the impact of SARS-CoV-2 on the nervous system.
'The prospect of COVID 19-induced brain damage has become a primary concern in cases of long COVID, but human neurons in culture are not susceptible to infection.' said lead author Professor Joseph Gleeson from the University of California San Diego School of Medicine. 'Prior publications suggest that the cells that make the spinal fluid could become infected with SARS-CoV-2, but other routes of entry seemed likely.'
Primarily a respiratory virus, SARS-CoV-2's long-term effects on the brain are not yet fully understood. The researchers, who have published their results in Nature Medicine, exposed the organoid to the virus. Using fluorescently tagged viral proteins and microscopy techniques they found that pericytes became infected. SARS-CoV-2 could then be produced by the pericytes, which served as 'replication hubs' aiding the spread of infection to other cell types, causing further damage. Interestingly, astrocytes, neural support cells, were the main target for secondary infection, leading to cell death.
Neural cell resistance to SARS-CoV-2 infection was also confirmed. When cortical organoids were exposed to the virus, fluorescent microscopy showed no changes in cell characteristics, as opposed to the pericyte based organoid. This reflects the findings of previous brain organoid and animal models which suggested that most neural cells have limited vulnerability for SARS-CoV-2 infection.
It is possible that the presence of angiotensin-converting enzyme 2 (ACE2) receptor containing cells is enough for infection. SARS-CoV-2 can use ACE2 as a receptor and this study found that blocking the ACE2 receptor with an ACE2 antibody partially prevented pericyte SARS-CoV-2 infection. Considering clinical and experimental data supporting ACE2 expression in pericytes, this model presents an alternative route to infection.
The authors explained that the results of this study implicate blood vessels as a potential route of brain infection by SARS-CoV-2. Infected pericytes can spread the infection to other types of brain cell, as well as cause blood vessel inflammation, followed by clotting, stroke or haemorrhages. Such complications are often observed in patients hospitalised with severe COVID-19.
The team has proposed the development of improved assembloids that contain pericytes and blood vessels capable of pumping blood in attempts to better model the human brain. Professor Gleeson commented that 'through these models greater insight into infectious disease and other human brain diseases could emerge.'





Leave a Reply
You must be logged in to post a comment.