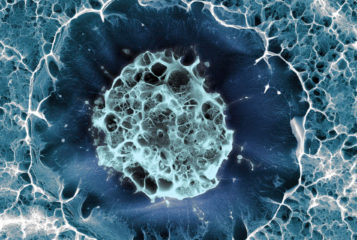
Altering the genetic makeup of immune cells could provide them with resistance to HIV, human immunodeficiency virus.
Researchers manipulated the genes of specialised immune cells called T cells before exposing them to HIV. The T cells showed significantly increased resistance to infection with HIV compared to those that had not been genetically altered.
'Providing an infected person with resistant T cells would not eradicate their viral infection. However, it would provide them with a protected set of T cells that would ward off the immune collapse that typically gives rise to AIDS', said co-author of the study Dr Sara Sawyer, from the University of Texas at Austin.
HIV attacks T cells by attaching to unique proteins found on their surface. Previous work has shown deactivating the gene for one of these proteins reduces the ability of HIV to infect T cells. Research published in Molecular Therapy extends this work, by additionally inserting genes known to be HIV-resistant.
Dr Matthew Porteus of Stanford School of Medicine, who co-authored the study, said: 'We inactivated one of the receptors that HIV uses to gain entry and added new genes to protect against HIV, so we have multiple layers of protection - what we call stacking'.
Using this technique the researchers were able to increase protection against the virus by more than 1200-fold, when compared to T cells that had not been genetically altered and which became infected within 25 days.
'HIV is a very nefarious and devious virus that likes to mutate and escape all the roadblocks we put in its way. So what we're trying to do is not just simply make one roadblock, but instead create several roadblocks', said Dr Porteus to CBS San Francisco.
Cutting and pasting multiple genes into the T cell genome provided the cells with a level of protection that increased with the number of HIV-resistant genes added. Cells with three HIV-resistant genes inserted showed greater protection than those with just one or two genes added.
HIV is known to rapidly mutate, so people infected must take a lifelong regimen of several drugs called highly active antiretroviral therapy (HAART), aimed at interfering with the virus at various stages of its lifecycle. 'Informally we actually call our method 'genetic HAART',' said Dr Sawyer. 'Instead of the cocktail of multiple drugs, we provide these cells with multiple antiviral genes'.
The method is labour-intensive and the process of inserting genes into a cell could lead to abnormalities such as cancer. Further research is therefore required before clinical trials can begin, which Dr Porteus hopes to start in three to five years.




Leave a Reply
You must be logged in to post a comment.