A toddler has become the youngest person to receive a bioengineered organ, receiving a life-saving windpipe transplant made from her own stem cells.
Hannah is two-and-a-half years old and was born with a rare congenital abnormality in which her trachea failed to develop. When she was born, a tube was inserted into her mouth so she could breathe on a ventilator.
The operation to transplant a windpipe into Hannah’s chest took nine hours and was performed by an international team of surgeons at the Children's Hospital of Illinois, US, headed by Dr. Paolo
Macchiarini of the Karolinska Institutet, Stockholm.
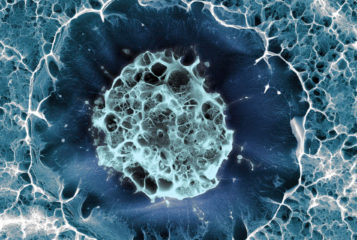
The team employed a two-step process to create the 'bioartificial' windpipe. Firstly, they engineered a 1.3 centimetre diameter synthetic scaffold out of plastic fibres using scans of Hannah’s chest as a template. This polymer tube had many tiny pores designed to support the growth of Hannah’s cells, promote a blood supply to the new organ and to degrade over time.
Secondly, the pores in and around the scaffold were filled with stem cells taken from Hannah’s bone marrow. This was achieved by mixing her stem cells with a supportive growth media in a bioreactor, where they could attach to the scaffold. Over approximately two days, the cells connected to the polymer, filling the pores and creating an organ.
'The transplant crosses frontiers by eliminating the need for a human donor and a lifetime of immunosuppressant drugs', said Dr Macchiarini. This is the sixth operation of this kind to be carried out by this international team (reported in 162874" title="<a href="http://www.bionews.org.uk /page_162874.asp">162874</a>" target="_blank" class="">BioNews 667). They now believe that this approach to building organs may work best with children, as it harnesses their natural ability to grow and heal.
It is hoped that regenerative medicine will one day be able to create more complex multi-tissue organs such as kidneys and lungs, but so far it has only been possible to grow and transplant basic, hollow organs such as bladders, bones and windpipes.
Hannah continues to recover and with the help of pulmonologists, respiratory therapists, and speech therapists, her future looks promising. 'Hannah's case is a great example of how the international community can work together to save a child's life', said Dr. Mark Holterman, co-surgeon and professor of surgery and pediatrics at the University of Illinois College of Medicine.
Sources and References
-
Toddler given life-saving windpipe transplant using her stem cells
-
First child in the world to receive tissue-engineered bioartificial trachea (press release)
-
Young Girl Receives Lifesaving Windpipe Transplant Made From Her Stem Cells
-
Groundbreaking Surgery for Girl Born Without Windpipe
-
Hannah’s Story — From Seoul to Peoria (press release)
-
Toddler Born Without a Windpipe Gets Artificial Trachea





Leave a Reply
You must be logged in to post a comment.