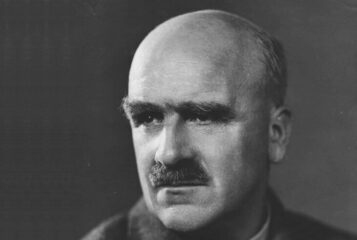
Gregor Mendel (1822-1884) was a scientist and monk whose Laws of Inheritance earned him the reputation of the 'father of genetics'. By observing patterns in pea plants, he helped revolutionise our understanding of biological inheritance and, consequently, human health and disease.
To celebrate Gregor Mendel's 200th birthday, the Progress Educational Trust (PET) and Genomics England held an event reflecting on what science and medicine have inherited from Mendel and what the future holds regarding our understanding and treating genetic disorders in the era of whole genome sequencing (WGS).
PET's director Sarah Norcross, chairing, kicked off the evening by asking: what are the prospects for understanding and treating Mendelian disorders in the era of WGS? And how are we addressing genetic conditions that do not follow Mendelian patterns of inheritance?
Dr John Parrington, associate professor of cellular and molecular pharmacology at the University of Oxford, gave a brief history of genetics and genomics which successfully set the tone and scene for the rest of the evening's presentations.
I enjoyed hearing how events unfolded from Darwin's theory of natural selection published in 1859 to the modern day. Dr Parrington explained how Mendel's work enhanced Darwin's insights by showing that certain 'factors', later called genes, could be inherited. I was surprised to hear that Mendel received little regonition for his work during his lifetime, and that it was only through the rediscovery of his research by others that it came to wider attention. After being introduced to Mendel's work by William Bateson, Sir Archibald Edward Garrod published the first account of a case of recessive inheritance in humans in 1902. And in 1933, Thomas Hunt Morgan won a Nobel Prize for discoveries elucidating the role of chromosomes in heredity. In 1983, Dr Barbara McClintock also won a Nobel Prize for discovering 'jumping' genes.
With just the right level of detail, Dr Parrington also explained how the Human Genome Project, which began in the 1990s, led to several discoveries. For example, only around two percent of the human genome codes for proteins, with the rest made up of so-called noncoding DNA, a fact which has deepened our understanding of epigenetics.
Following this, Dr Gemma Chandratillake, chair of the British Society for Genetic Medicine and of the Cambridge Rare Disease Network, delved into medical genetics. Dr Chandratillake gave a compelling argument as to why genetic diagnosis is often necessary, explaining the importance of providing a faster route to accurate diagnosis, thereby giving people closure, more choice and the ability to make informed decisions. She also spoke about the development of personalised medicines and the rapid rise in pharmacogenetics, with the ultimate goal of being more intelligent about the medication clinicians prescribe. She briefly touched on some ethical issues around data sharing, and said that genomics alone could not produce great healthcare. It needs to be effectively embedded into care pathways to benefit patients.
This led seamlessly into the following talk by Angela Douglas, deputy chief scientific officer at NHS England. Douglas described the UK as a world leader in genomic medicine thanks to the long, rich history of genomics in the NHS, starting in the 1950s. She spoke positively about the unique structure of the NHS and how it can deliver at scale and pace. She praised the work of the Genomic Medicine Service and outlined the important lessons learned from the 100,000 Genomes Project.
Writer, broadcaster and head of engagement at Genomics England, Vivienne Parry's account of how the 100,000 Genomes Project came about was entertaining and surprising. I had no idea that when David Cameron announced the project in 2012, no one knew if it was even possible. Parry explained that while the sequencing and analysis turned out to be less problematic than expected, making it work in a healthcare system was far more challenging.
I also liked Parry's take on public engagement, saying that this is not about education or persuading people what to do, but rather about giving them the correct information to make their own choices. She emphasised the need for clear messaging delivered through the proper channels, and likened this to vaccine confidence, with attention paid to talking, listening and maintaining an open dialogue. Her final message was about the importance of collaboration between industry and professional organisations. She warned against the dangers of poor messaging around genetic technology, referencing Monsanto and its messaging around its GMOs as an example of what not to do.
The final talk of the evening came from Dr David Bick, clinical adviser at Genomics England's Newborn Genomes Programme. He spoke about the existing shortfalls of the current newborn screening programme and how WGS could help to overcome these, with the main benefit of increasing the number of genetic conditions screened for. He also briefly mentioned the recent public dialogue on the topic. It was encouraging to hear that there is interest and receptivity among the general public.
Dr Bick also made a valid point about needing to engage minority groups to ensure there's no bias and everyone has access to the same services. For a more in-depth discussion, I'd recommend PET's five-part series WGS at Birth which can be viewed on PET's YouTube channel.
The Q&A with the audience started with a common question about the cost of WGS. Douglas gave a figure of £150 per test and said that maximising the number of samples sequenced per day could bring the price down further. Parry put the cost into perspective, saying that an MRI costs approximately £600.
Other questions concerned how we can ensure that those with genetic conditions are valued in society, and whether WGS is actually necessary. Dr Chandratillake said it is essential that we listen to the voices of those with genetic conditions, to get a better sense of their needs and concerns. Dr Parrington said it was a delicate question, and that we should not always equate diagnosis with disease or disability, saying that some conditions can involve an entire spectrum of attributes and experiences.
Regarding the need for WGS, Dr Bick discussed the difficulties of trying to screen using multiple tests. For example, mass spectrometry analysis requires taking numerous samples from the same blood spot, limiting the number of tests. He also mentioned that WGS could add 200-300 more conditions to the existing list of conditions screened. He briefly discussed the sensitivity and specificity of WGS, but said these were topics for another time.
The final and most provocative question of the evening was 'When will all newborns and adults have their whole genome sequenced?'. Dr Parrington said he hoped this might happen soon, but it could only happen if we address a number of related ethical issues and gaps in our understanding. Douglas agreed with this, and said she hoped WGS would come to be offered much more widerly during the next 20 years.
Dr Chandratillake took a slightly different direction, and said that we would never be in a situation where absolutely everyone had their whole genome sequenced, as this should always be a choice and some will always opt out. Parry agreed, saying the information gained from research would be enough to develop routine tests, and avoid the need to sequence the genomes of absolutely everyone. She ended on a comical note, saying that there are still many unknowns and complexities, and that while humans have a similar number of genes to a starfish they are somehow not starfish.
PET is grateful to Genomics England for supporting this event.





Leave a Reply
You must be logged in to post a comment.