Mini organs are being developed from stem cells to study how SARS-Co-V2 affects the body.
According to an article written in Nature News, studies have demonstrated that the virus infects lung, liver and kidney tissue grown in the lab, which explain the complications in patients with COVID-19. Furthermore, Nature News reports that researchers are also studying the effects of drugs in these mini organs to test if they could be used as new therapies.
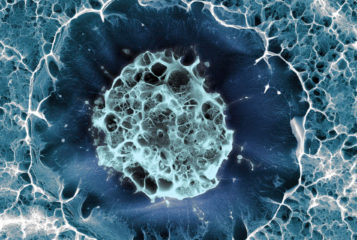
Mini organs, called organoids, are derived from stem cells and can be used to replicate the complexity of organ tissues. Unlike cell lines grown in a dish they 'resemble the true morphology of tissues,' Professor Thomas Efferth, a cell biologist at Johannes Gutenberg University of Mainz, Germany, not involved in the studies, said.
It is unclear whether the effect of COVID-19 on different organs is directly related to the coronavirus infection itself or to secondary effects due to an excessive immune response. The use of organoids as a tool can help understand how the coronavirus travels, which organs are affected and what damage it does.
One of the insights from using this model was the discovery that the virus infects the cells lining the blood vessels, which allows the viral particles to integrate in the blood from the lungs and spread throughout the body affecting other organs. 'Pathology reports of damaged blood vessels in people with COVID-19 also support this hypothesis', said Dr Josef Penninger, a genetic engineer at the University of British Columbia in Vancouver, Canada, and co-lead author of this study.
The virus has also been shown to directly infect the kidney, liver and gut organoids. 'We are fairly confident now that the virus that causes COVID-19 can infect tissue outside the lung and significantly contribute to disease,' said Dr Penninger. However, researchers are not certain if the infection of these organs exclusively result in the symptoms present in COVID-19 patients. Probably, more severe implications in patients are due to a combination of viral infection and immune responses.
Organoids are also being studied to determine whether they are good models to test COVID-19 therapies. This could add a layer of confidence in a drug's efficiency before it is tested in clinical trials.
'We will only know at the end of this process what the predictive value of these systems are for testing drug efficacy,' said Dr Bart Haagmans, a virologist at Erasmus MC in Rotterdam, the Netherlands, who developed the gut organoids. 'This is a long-term process.'
Organoids do, however, have limitations, as they cannot reflect the crosstalk between organs in the human body. Therefore, the studies will need to be validated in animal models and human clinical trials.




Leave a Reply
You must be logged in to post a comment.