Female infertility gets a great deal of airtime. From posters on the tube, to dramatic headlines with declarations of 'fertility falling off a cliff at 35 years of age', it's very clear that most of the public awareness around infertility focuses on women.
But this is only telling half the story. A historic lack of investment in targeted treatments means that male infertility hasn't received the attention necessary to raise awareness, open up the conversation, or provide therapeutic options that focus on the cause. More recent media have aimed to break the stigma associated with male infertility: a documentary hosted by comedian Rhod Gilbert (see BioNews 1083) and interviews with Love Island star Chris Hughes (see BioNews 1072) have begun to shed light on a previously neglected topic, but the lack of therapeutic options remains a challenge for individuals and couples facing fertility issues.
With this in mind, last week's online event 'What's in the Pipeline for Male Infertility' provided some much-needed insight into ongoing research into the causes and possible treatments for male fertility issues. The event was produced by the Progress Educational Trust (PET), the charity that publishes BioNews, and was supported by the Scottish Government. It was chaired by PET's director Sarah Norcross and featured speakers from the UK and USA, each working on different aspects of the male infertility story.
Norcross opened the event by providing some context on what current treatment looks like for male infertility. I was surprised to learn that the only regularly offered treatment option for male infertility is ICSI (intracytoplasmic sperm injection), which involves injecting sperm directly into an egg prior to normal IVF embryo transfer. However, ICSI is not a guaranteed route to pregnancy despite being offered as a 'catch-all' for many underlying causes of male infertility. So, what can we do to investigate and treat instances of male infertility, without requiring women to undergo a very invasive treatment that might not result in a successful pregnancy?
First to speak was Dr Sarah Martins Da Silva, senior lecturer in systems medicine at the University of Dundee. Dr Martins Da Silva, who was recently interviewed by Norcross for BioNews (see BioNews 1098), began her talk by explaining the underlying causes of male infertility, and how current therapeutic options (namely ICSI) fall short of providing a reliable solution. She then moved on to discuss the work she is currently involved with, investigating the importance of a protein called phospholipase C zeta (PLC zeta) in egg activation. Work by Dr Martins Da Silva and her team has found that sperm that are deficient in PLC zeta are linked to some instances of male infertility, likely due to a failure of egg activation at the point of fertilisation. By tackling this underlying issue, Dr Martins Da Silva has found that combining ICSI with an assisted egg activation technique – in instances where sperm is found to be low in PLC zeta – can result in improved fertilisation and successful pregnancy outcomes compared to ICSI alone. Focusing on PLC zeta might not be a universal solution, but the work presented by Dr Martins Da Silva shows it has a role as a therapeutic target when investigating male infertility in the future.
Next was Jamie Chorlton, head of clinical development for St George Street Capital, a charity that accelerates clinical trials for drugs with the potential to help patients with unmet needs. One of their current focuses is idiopathic male infertility (IMI) - cases of infertility in men which result from an unexplained reduction in sperm quality. As Chorlton explained, 80 percent of IMI cases have indicators of oxidative stress in semen. By reducing the activity of a pro-oxidant enzyme called myeloperoxidase (MPO), the levels of reactive oxygen species in sperm decreases, which in turn increases sperm quality and can lead to improved fertility. It is hoped that upcoming trials arranged over a three-year period by St George Street Capital will show if taking an MPO inhibitor can improve sperm quality and fertility. If successful, this preliminary work will see the drug licensed back to the original developer for further trials, with the potential for clinical application in instances of male infertility in the future.
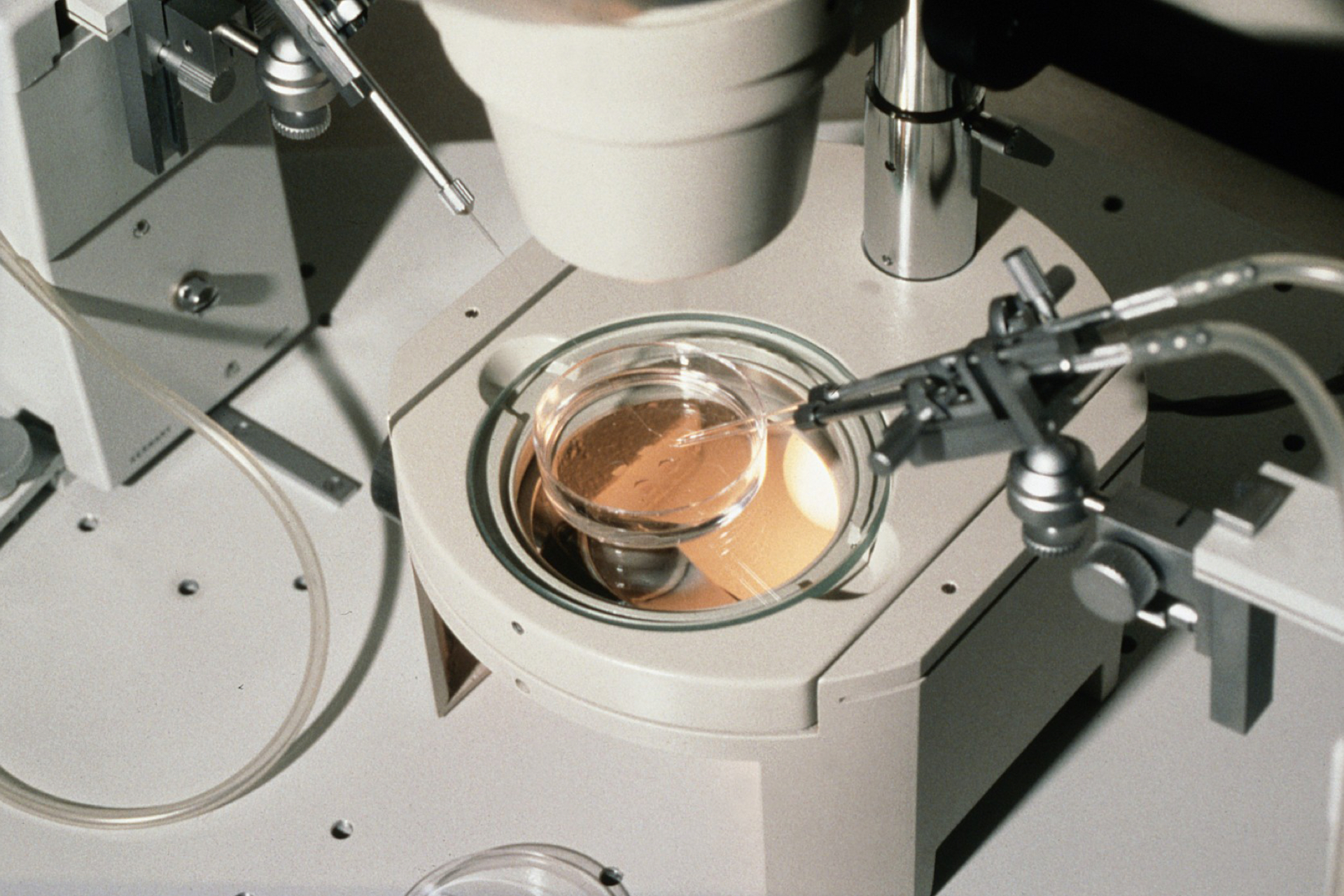
The final two talks covered two areas of male infertility that have historically not been a priority: diagnosing male fertility from sperm samples, and pre-emptively treating male infertility as a result of cancer treatment in young men. Dr Tiffany Wood, founder and CEO of Dyneval, spoke about a tool she has developed based on complex fluid properties and how this can aid in sperm diagnosis. Methods for assessing semen have not improved for many years and rely on a slow, manual process. Previous forays into computer-aided semen analysis have been quite hit-or-miss, given their reliance on high concentrations of semen samples. As Dr Wood explained, Dyneval technology has already been successfully applied in agriculture settings and animal reproduction. By working with human fertility scientists (including Dr Martins Da Silva), it is hoped that Dyneval might also be used to assess sperm quality and health in a clinical setting too.
Lastly, Professor Robert Brannigan, from the Department of Urology at Northwestern University, Feinberg School of Medicine, Illinois, spoke about the importance of developing and applying methods that might aid male fertility after cancer treatment. This was something that I had previously read about for young female cancer patients, but it was the first time I had heard about such measures being used to preserve fertility in men. Professor Brannigan explained that although the cryopreservation of sperm is an existing approach, cryopreserving testicular tissue prior to cancer treatment is an emerging technology with the potential to aid fertility in pre-pubescent patients.
Overall, it was interesting to see infertility being explored from a new perspective, and encouraging that many different approaches are being taken to understand the problem in a clinical setting.
Norcross then invited the audience to ask the put questions to the panellists. Many questions came from people looking for treatment options for male infertility, which emphasised how important the work being undertaken in this area is, and how it can impact upon lives on a personal level. As research progresses and the conversation about male infertility opens up, there are exciting prospects for improved treatments and earlier intervention.
PET is grateful to the Scottish Government for supporting this event.



Leave a Reply
You must be logged in to post a comment.