Three separate clinical trials of engineered immune cells have reported results for treating glioblastoma, an aggressive and hard-to-treat brain cancer.
All three teams deployed next-generation engineered T-cells called chimeric antigen receptor T (CAR-T) cells to treat patients with glioblastoma. A team from the City of Hope Cancer Centre in Duarte, California, was among the first to publish their results in Nature Medicine. The other teams from the University of Pennsylvania and Massachusetts General Hospital, both using a dual-targeting approach, publishing a week later in Nature Medicine and the New England Journal of Medicine respectively. All described their pioneering CAR-T designs.
'The CAR-T platform has revolutionised how we think about treating patients with cancer, but solid tumours like glioblastoma have remained challenging to treat because not all cancer cells are exactly alike and cells within the tumour vary. Our approach combines two forms of therapy, allowing us to treat glioblastoma in a broader, potentially more effective way,' said Dr Bryan Choi, lead author of the study from Massachusetts.
Professor Donald O'Rourke, lead author of the study from Pennsylvania, said '… [we] are eager to continue our trial, which will give us a better understanding of how this dual-target CAR-T cell therapy affects a wider range of individuals with recurrent glioblastoma… This cancer is unique in each individual, so a wider range of patients will help us determine the optimal dose, better understand effects like neurotoxicity, and more firmly establish efficacy.'
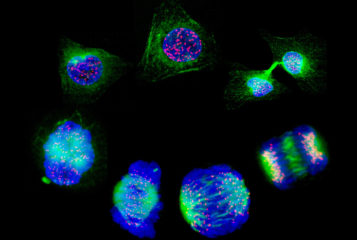
CAR-T cell therapy harnesses the patient's own immune system to combat cancer. T-cells, which are responsible for identifying and combating infections and diseases, are extracted from the patient and genetically modified to recognise specific molecules (antigens) that are exclusively found on the tumour cells. The CAR-T cells are then injected back into the patient.
Glioblastoma is the most common and aggressive form of brain malignancy in adults. It is incurable, with treatment a significant challenge due to their rapid growth and tendency to infiltrate healthy brain tissue, forming diffuse tumours that are difficult to remove surgically.
The Massachusetts team designed CAR-Ts to bind to both wildtype EGFR (the receptor for the hormone epidermal growth factor which drives cell proliferation) and a common cancer mutation of EGFR. The dual approach helped the cells home in on tumours for more effective tumour killing. The therapy resulted in a rapid response in the first three patients treated, but disease recurrence eventually occurred in all.
The Pennsylvania team also deployed a double targeting approach, whereby the CAR-T cells were engineered to bind EGFR and another antigen commonly over-expressed in glioblastoma, IL13Rα2. Researchers found that within 48 hours after CAR-T cells were injected directly into the cerebrospinal fluid, the tumour reduced in all six patients treated. Some patients remained progression free for over six-months.
The City of Hope study, lead by Professor Christine Brown, is the largest reported trial to date of CAR-T therapy for solid tumours, which included 65 patients with recurrent glioma brain tumours. They used CAR-T cells that solely targeted IL13Rα2, the same antigen targeted by the Pennsylvania team.
The primary aim of the trial was to evaluate feasibility and safety. Three routes of administration were evaluated: direct injection to the tumour site, infusion into the cerebrospinal fluid or injection into both areas. Doses of the therapy were escalated as the trial progressed and all doses tested and all routes of delivery were well-tolerated.
The study saw half of the patients achieved stable disease for at least two months following treatment, two patients demonstrated partial response and two other patients showed complete response, where their tumours disappeared after treatment.
Peter Valadez is one of the patients who achieved complete remission. Diagnosed with a high-grade glioma in 2014, he underwent three surgeries and radiation therapy before receiving CAR T-cell therapy in 2018. '[One doctor] told me to look into receiving CAR-T cell therapy at City of Hope. I did, and that is why I am still here today,' said Valadez.
Despite the recurrence of glioblastoma in some patients in the three trials, researchers are hopeful the initial positive response to CAR-T treatment will continue to pave the way for more effective and safe therapies for hard-to-treat cancers like glioblastoma.
Sources and References
-
Deadly brain cancer shrinks after CAR-T therapy - but for how long is unclear
-
'Dual-Target' cell therapy appears to shrink brain tumours, Penn Medicine research finds
-
Intrathecal bivalent CAR T cells targeting EGFR and IL13Rα2 in recurrent glioblastoma: phase 1 trial interim results
-
Preliminary clinical trial results show 'dramatic and rapid' regression of glioblastoma after next generation CAR-T therapy
-
Intraventricular CARv3-TEAM-E T cells in recurrent glioblastoma
-
City of Hope-developed chimeric antigen receptor (CAR) T cell therapy shows clinical activity in patients with aggressive brain tumors in a Phase 1 trial
-
Locoregional delivery of IL-13Rα2-targeting CAR-T cells in recurrent high-grade glioma: a phase 1 trial
-
Living drugs that reprogram patients’ immune cells show early promise against hard-to-treat brain tumors




Leave a Reply
You must be logged in to post a comment.