A 13-year-old girl has received the first ever 'base-editing' therapy, in which cells were genetically modified to fight her otherwise incurable leukaemia.
Researchers at Great Ormond Street Hospital (GOSH) in London recently reported on this landmark from their ongoing phase I trial, which is the first to use this method clinically. This work builds on previous results from the same group who have pioneered using novel genetic and cellular therapeutic techniques, including the recent publication of an 'off-the-shelf' cellular therapy for B cell leukaemia. This trial considers rarer and harder-to-treat T cell leukaemias, using a similar technique of making 'chimeric antigen receptor T cells' (CAR-T cells) capable of recognising and destroying cancer cells.
'This is a great demonstration of how, with expert teams and infrastructure, we can link cutting-edge technologies in the lab with real results in the hospital for patients' said Professor Waseem Qasim, consultant immunologist at GOSH and programme lead. 'It's our most sophisticated cell engineering so far and paves the way for other new treatments and ultimately better futures for sick children'.
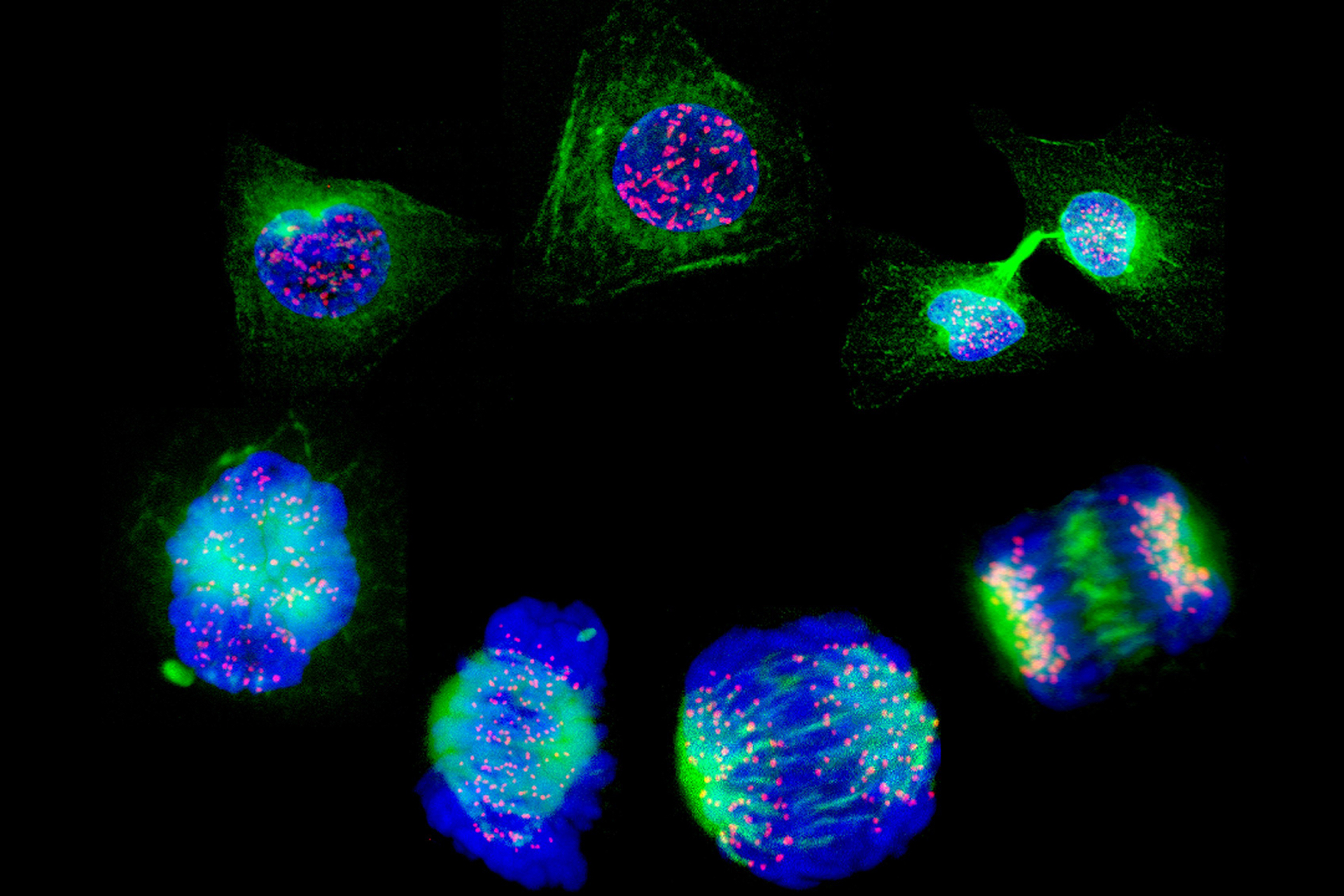
The base-editing technology is a refined version of the CRISPR/Cas9 method used to modify T cells in the earlier study. Developed by researchers at Harvard University, Cambridge, Massachusetts, base-editing involves engineering the Cas9 enzyme to chemically change the DNA bases ('letters') at specific sites. This avoids some of the problems and risks that come with regular CRISPR/Cas9 editing, which relies on physically cutting the DNA backbone.
Base-editing is used here to remove three unwanted genes from donated T cells: one that is expressed on T cells (CD7), and two others that allow donated cells to get safely established in the recipient's body (TRAC and CD52). Then a CAR that recognises CD7 is added, and the engineered cells can be given to a patient with T cell leukaemia, where they will kill the cancerous T cells but not themselves.
Before becoming the first patient to be enrolled on this trial, Alyssa had already undergone all standard-of-care therapies for her leukaemia, none of which worked. It took a month for her cancer to go into remission after receiving the base-edited CAR-T cells, at which point she was able to receive a bone marrow transplant to give her a working immune system. That was six months ago: she is reportedly recovering well at home.
Base editing is being used in this trial to completely prevent certain genes being expressed, however as Dr David Liu, co-inventor of the technology, told the BBC: '… therapeutic applications of base editing are just beginning'.
Base editing could be used to change a person's DNA at a particular site to change – not remove – expression of a particular protein. Many diseases that are caused by single bases in a person's DNA might be treatable with this technology; biotech-led trials are already ongoing for sickle cell disease and a form of hereditary cardiovascular disease.
Sources and References
-
GOSH patient receives world-first treatment for her 'incurable' T-cell leukaemia
-
World-first use of base-edited CAR T-cells to treat resistant leukaemia
-
Experimental CRISPR technique has promise against aggressive leukaemia
-
CAR T cells to fight T cell leukaemia
-
Base editing: Revolutionary therapy clears girl's incurable cancer




Leave a Reply
You must be logged in to post a comment.