Adults with thalassemia, a severe genetic blood disorder, will be offered potentially curative stem cell transplants on the NHS for the first time.
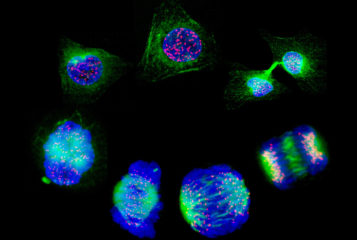
Adults living with transfusion-dependent thalassemia in the UK currently rely on regular blood transfusions to manage their symptoms and survive. The new treatment, known as an allogeneic haematopoietic stem cell transplant (Allo-HSCT), involves replacing the patient's blood stem cells with those of a matched sibling donor. Previously, this treatment was only available to children due to an increased risk of complications in adults. However, due to advances in transplant treatments, the use of Allo-HSCT can now be extended to adults, with an estimated 600 adults eligible for the new treatment.
Professor Sir Stephen Powis, NHS England medical director, said: 'Expanding the availability of stem cell transplants to adults living with thalassaemia is another vital step forward to help change the lives of those living with this deeply debilitating condition. Thalassaemia can be an incredibly painful condition with difficult symptoms for patients as well as the impact on their heart, liver and bones, and it's fantastic that offering this evidence-based curative stem cell treatment can now offer new hope to help significantly improve patients' quality of life.'
Thalassaemia is a genetic condition that affects the production of haemoglobin, an essential blood molecule that helps red blood cells carry oxygen around the body. Previously, transfusion-dependent thalassaemia, which is a severe form of the condition, was previously fatal in childhood. Yet, with blood transfusions every two to four weeks' patients are now able to survive into adulthood.
Relatedly, a CRISPR-based gene therapy (known as Casgevy) for transfusion dependent thalassaemia was recently authorised by the UK medicines regulator, with the treatment currently under review by the National Institute for Health and Care Excellence (see BioNews 1216).
However, genome editing is not used in Allo-HSCT, which is more commonly known as a bone marrow transplant. Yet, this treatment is also not without risk, as the patient must firstly undergo chemotherapy and radiotherapy to wipe out their immune system. Afterwards, their immune systems are rebuilt using blood stem cells from a matched-sibling donor that are harvested before treatment. The stem cells are given to the patient via an intravenous infusion to re-establish healthy blood cell production.
'We celebrate the long-awaited approval of Allo-HSCT for adults with transfusion dependent thalassaemia. This remarkable milestone offers hope to adults with donor matches who were previously excluded from accessing a curative option.' Romaine Maharaj, UK Thalassaemia Society executive director, said 'While it is a huge step in the right direction and a monumental win for thalassaemia, we also eagerly await the much-needed approval for gene therapies. Having both curative options available will grant more patients the chance to live transfusion-independent lives, enhancing both their quality of life and life expectancy'.
Sources and References
-
NHS to offer stem cell transplants to cure life-limiting blood disorder
-
Thalassaemia: NHS to offer stem cell transplants to adults who need transfusions
-
Transplants to cure life-limiting disorder
-
NHS to offer stem cell transplants to patients living with rare blood disorder
-
Stem cell transplants now available on NHS for adults with thalassaemia




Leave a Reply
You must be logged in to post a comment.