A gene therapy treatment for sickle cell disease has led to a build-up of cells with genetic mutations that make them grow faster, increasing blood-cancer risk, researchers revealed.
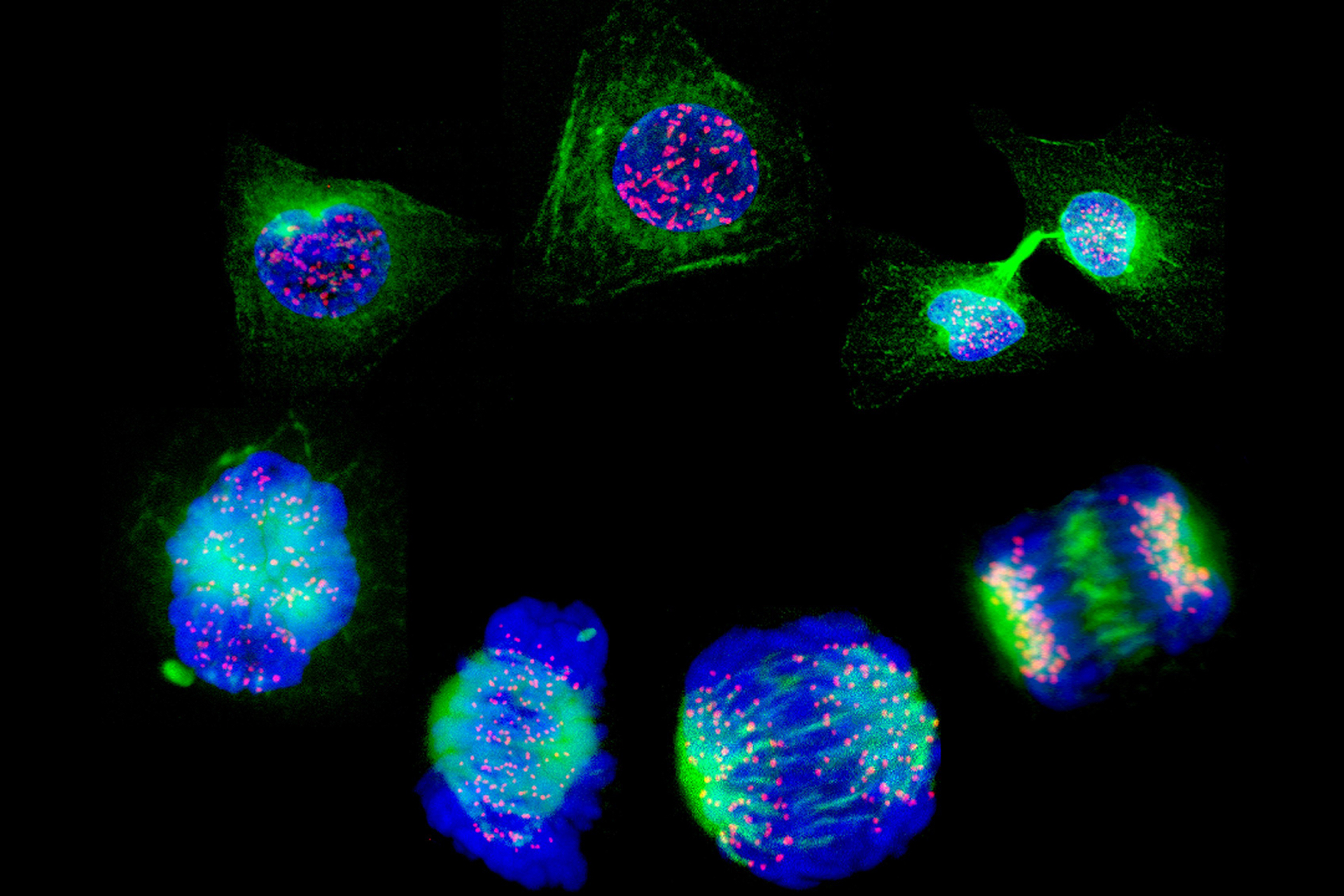
An international research team, led by the University of York, analysed blood cell samples from six patients with sickle cell disease who were undergoing gene therapy as part of a clinical trial at Boston Children's Hospital. Using whole-genome sequencing, the scientists tracked and compared DNA changes in the patients' stem cells before and after gene therapy. They discovered post-treatment there was an accumulation of stem cells with DNA mutations that enhance cell growth and proliferation. These mutations are associated with blood cancers, such as leukaemia, and are also more commonly found in elderly individuals, as genetic mutations accumulate across a lifetime. The study has also shown that younger patients, who have accumulated fewer genetic mutations, did not show the same increase in mutations after the treatment.
Publishing their findings in Nature Medicine, co-senior author of the study, Professor David Kent from York Biomedical Research Institute, said 'Our research indicates that... after gene therapy, the treatment might favour growth of stem cells with certain mutations, and this in turn could potentially lead to expansion of blood cells containing these mutations. In other settings, such expansions have been associated with development of blood cancers, particularly in older individuals, but the relationship of this study's findings to the risk of blood cancers is not yet fully understood.'
Sickle cell disease is a genetic disorder that results in abnormal 'sickle' shaped red blood cells in contrast to round disc shaped cells in healthy individuals. These cells are less capable of carrying oxygen and may block blood vessels, causing severe complications. Patients often require lifelong blood transfusions and until recently the only cure was stem-cell transplantation.
The approach to gene therapy used in the clinical trial implicated in this study is different to the approach used in the development of Casgevy (see BioNews 1216), which uses the genome-editing approach CRISPR to treat sickle cell disease. Both target the BCL11A gene in order to switch on the production of fetal haemoglobin, however this clinical trial used a new design called a shimiR vector, where genetic material is delivered via a lentiviral vector to the cells.
The study suggests that the treatment itself does not cause the mutation, but rather the ex vivo process of editing the cells outside the patient's body, followed by re-transplantation.
Dr David Williams, from Boston Children's Hospital and Harvard Medical School, Massachusetts and co-senior author of the study, told BioNews... 'while we report on work done in our own trial, you will see the implications are broader. Other trials have not done this depth of analysis. We believe this has implications for any ex vivo manipulation (genome editing, viral vectors) and could in fact have implications for any therapy that requires expansion of haematopoietic stem cells in sickle cell disease patients.'
This study highlights the need for long-term and in-depth studies to monitor patients undergoing gene therapies in order to fully understand their safety.
A multi-site National Institutes of Health and California's Stem Cell Agency funded phase 2/pivotal trial is currently underway.
Sources and References
-
New research sheds light on cancer risk in gene therapies
-
New research advances understanding of cancer risk in gene therapies
-
Clonal selection of hematopoietic stem cells after gene therapy for sickle cell disease
-
Sickle cell gene therapy process may cause cancer-linked mutations in blood stem cells


Leave a Reply
You must be logged in to post a comment.