A technique commonly used to amplify minute quantities of DNA to allow genetic testing of early human embryos has been shown to be error-prone. Potentially harmful unintended mutations in genome-edited embryos were also found.
The study, published in Nature Communications, showed that when a technique called whole genome amplification (WGA) was used in single-cell genome sequencing, more than a quarter of genes previously confirmed to be heterozygous were inaccurately labelled as homozygous. WGA is commonly used in embryo genome editing research and in preimplantation genetic testing, where only tiny amounts of DNA are available.
'Whole genome amplification has limitations that reduce the accuracy of genetic testing. The concern is that we might be misdiagnosing embryos' said Professor Paula Amato, senior co-author and professor of obstetrics and gynaecology at Oregon Health and Science University (OHSU). However, she added, 'pre-implantation genetic testing using more advanced technology is still clinically useful for detecting chromosomal abnormalities and genetic disorders caused by a single gene mutation transmitted from parent to child'.
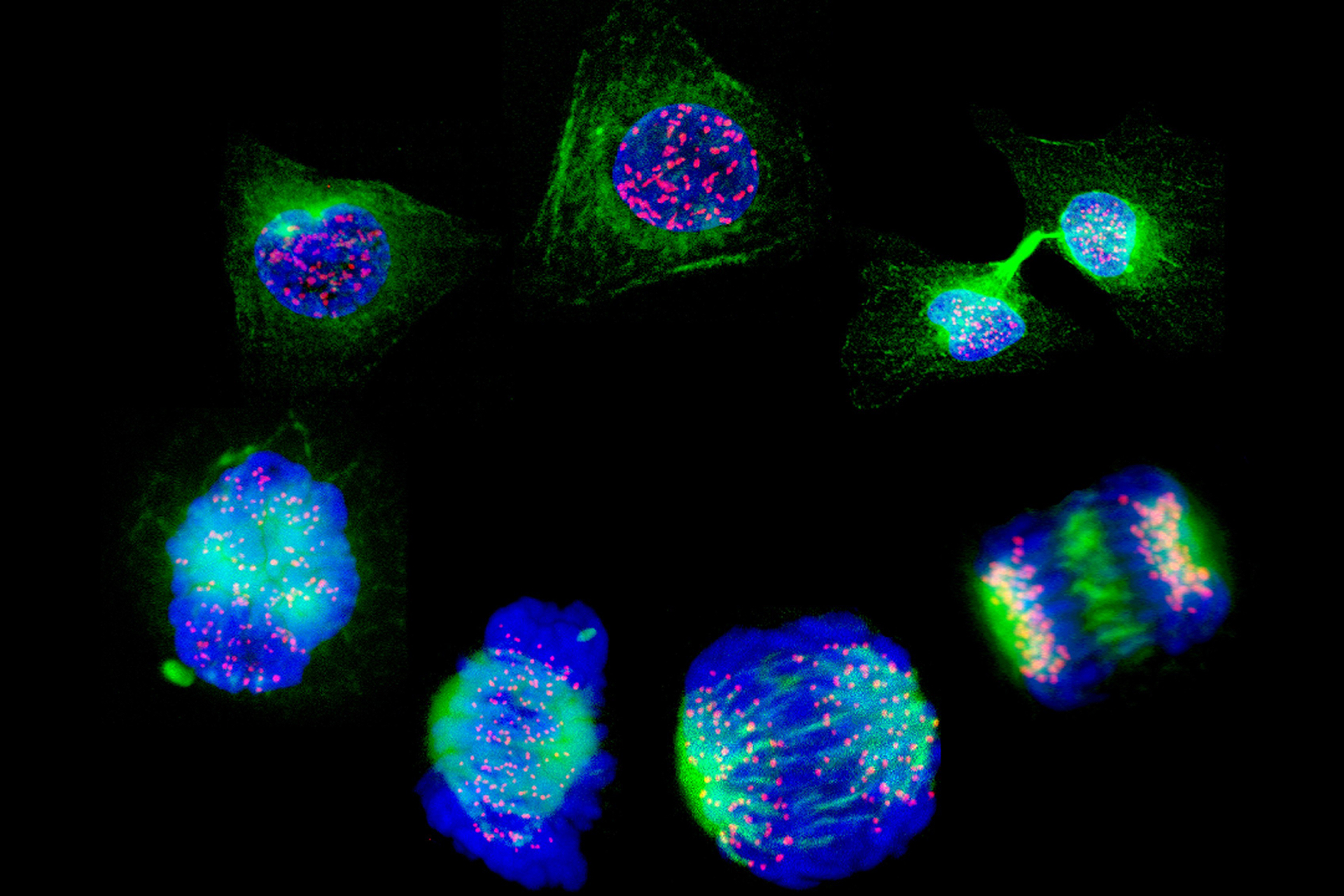
Researchers then investigated embryonic stem cell lines (ESCs) from genome-edited embryos to overcome the need to use WGA. ESCs can multiply indefinitely, and can supply enough DNA for analysis without requiring amplification.
Previous research from the same lab showed that a process known as gene conversion occurs regularly in early human embryos following a double-strand break in their DNA. The embryos repair these breaks, using the normal copy of the gene from the other parent as a template.
In the current study, the scientists used CRISPR/Cas9 genome editing to induce a double-strand break in DNA at the precise site of a mutation. In doing so, they confirmed the gene conversion repair mechanism.
However, genome sequencing revealed that unintentional and potentially harmful changes occur in the genome from the gene conversion repair mechanism, when copying the gene from one parent to correct the disease-causing mutation from the other parent.
During this process, loss of heterozygosity occurs. The repairing mechanism creates an identical genetic sequence extending from the DNA breakpoint using the allele of a particular gene from one parent, reducing heterozygosity. This results in an increased risk of recessive disease, and can lead to certain cancers, where tumour suppressor genes are absent or non-functional.
Senior co-author Professor Shoukhrat Mitalipov, director of OHSU Centre for Embryonic Cell and Gene Therapy, discussed these findings in a presentation at the Third International Summit on Human Genome Editing, which took place last week at the Francis Crick Institute, London.
Professor Mitalipov explained that correcting a disease-causing mutation in early human embryos may create more problems than it solves. 'If you're cutting in the middle of a chromosome, there could be 2000 genes there… You're fixing one tiny spot, but all these thousands of genes upstream and downstream may be affected.'
'It tells you how little we know about editing the genome, and particularly how cells respond to the DNA damage that CRISPR induces,' concluded Professor Mitalipov. 'Gene repair has great potential, but these new results show that we have a lot of work to do.'



Leave a Reply
You must be logged in to post a comment.